Cook Islands Natural Heritage Articles
Dengue - A Complex Disease
Dengue Fever epidemics have been reported in the tropics of Africa, Asia and the Americas since 1780. It was a non-fatal disease with a very high fever and intense joint/muscle pain.
It was not until the 1950s, in Southeast Asia, that dengue became associated with fatalities. The illness was like classical Dengue Fever (DF) except that, instead of recovering as the fever subsided, a few patients experienced severe bleeding (haemorrhage), and these were said to have developed Dengue Haemorrhagic Fever (DHF). This severe haemorrhagic form of dengue developed mainly among patients under 20 years of age. The haemorrhagic form of dengue did not appear in the Americas until 1981 during an epidemic in Cuba.
Both forms of dengue (DF and DHF) have dramatically increased throughout the tropics in the last twenty years. WHO estimates that there are now more than 50 million cases-a-year of the milder classical Dengue Fever, and more than 500,000 develop the severe Dengue Haemorrhagic Fever. If untreated, DHF has an mortality of about 20%, but with correct treatment  it is less than 0.5%. The two forms of dengue are caused by the same virus, and that virus is spread by day-biting Aedes mosquitoes, especially Aedes aegypti.
it is less than 0.5%. The two forms of dengue are caused by the same virus, and that virus is spread by day-biting Aedes mosquitoes, especially Aedes aegypti.
There are four types (serotypes) of the dengue virus: Dengue-1, Dengue-2, Dengue-3 and Dengue-4. The numbers reflect the order of discovery, and have nothing to do with severity of the disease. Each serotype has been known to cause the severe haemorrhage of Dengue Haemorrhagic Fever (DHF) in some patients, and to have caused some fatalities. It is not known why some epidemics have more severe haemorrhage cases than others.
Who called it Dengue?
In Africa there was a disease known in Swahili as dinga, or ka dinga pepo. This disease went with the slaves to the Americas, where there was a notable epidemic in Cuba in 1827. The name dinga was popularly (and incorrectly) identified with the Spanish word dengue, meaning “fastidious”, and this became the name of the disease in the United States and the English speaking world. It is usually pronounced as “deng-ee”. Other early names were Breakbone Fever, reflecting the intense joint/muscle pain, and Dandy Fever, reflecting the stilted movement of patients.
Spread by mosquitoes
 The dengue virus is spread by Aedes mosquitoes. On Rarotonga we have two Aedes mosquitoes and both are spreaders: the Dengue Mosquito (Aedes aegypti ) and the Polynesian Mosquito (Aedes polynesiensis). The males and females live on any sugary-juice from plants, although the female requires blood-meals to develop her eggs. The Dengue Mosquito is highly domestic and breeds in mainly artificial containers of water, especially dark-coloured containers with wide openings in shaded areas. The Polynesian Mosquito also breeds in containers around dwellings, but can also breed in small water-holes throughout the lowland and the mountains.
The dengue virus is spread by Aedes mosquitoes. On Rarotonga we have two Aedes mosquitoes and both are spreaders: the Dengue Mosquito (Aedes aegypti ) and the Polynesian Mosquito (Aedes polynesiensis). The males and females live on any sugary-juice from plants, although the female requires blood-meals to develop her eggs. The Dengue Mosquito is highly domestic and breeds in mainly artificial containers of water, especially dark-coloured containers with wide openings in shaded areas. The Polynesian Mosquito also breeds in containers around dwellings, but can also breed in small water-holes throughout the lowland and the mountains.
The day-active female mosquitoes suck viruses from an infective person and the virus multiplies within the mosquito without affecting her health. In 3-15 days (typically 8-11 days) the virus spreads into her salivary glands and, for the rest of her life, she will inject a few viruses each time she takes a blood-meal. An Aedes aegypti female mosquito typically seeks two or three blood-meals a week, lays eggs once a week, and lives for about two months. Aedes are not long-distance fliers and usually remain within 100 metres of where they hatched.
The life cycle of a mosquito: it takes 7-12 days (depending on temperature) to develop in water from the egg, through larvae (“wrigglers”) and pupa (“tumblers”) stages to emerge as flying adults. Under favourable conditions a young female mosquito can undertake her once-a-life mating and find a blood-meal within a day, and lay her first eggs a couple of days later.
The young female mosquito is virus-free until she sucks blood from person with dengue at an infective stage - the first 4-5 days of actual fever. Other mammals, such as dogs and pigs, do not get infected, nor do they transmit the viruses to mosquitoes. Neither Aedes aegypti nor A. polynesiensis transmit the dengue viruses through the eggs to their offspring, and mating males do not transfer the viruses to other females. Newly emerged adult mosquitoes can only get dengue viruses from an infective person.
A mosquito without dengue viruses in her salivary glands can sometimes transmit the virus mechanically. If she is interrupted while feeding on an infective person she might immediately continue her blood-meal from a another person and directly transfer some of the viruses that are on her mouthparts.
After a person is infected, the dengue viruses incubate unnoticed for 3-14 days (usually 4-6 days), and then the fever develops. A person is infective to mosquitoes for the first 4-5 days of the illness.
Immunity and vaccines
A virus is not living, like a bacteria, and it therefore cannot be killed with antibiotics. The infection is finished when your immune system finally makes: (1) antibodies that can recognise and inactivate viruses floating in your blood; and (2) white cells that can recognise and engulf virus-infected cells. After the immune system has been successful, it never forgets the virus and you are immune for life. What makes the dengue virus especially successful is that there are four types and, when you have dengue, you develop a life-long immunity to that one type only. You are therefore still susceptible to the other three types of dengue.
A vaccine contains inactivated viruses or essential virus-parts to trigger the immune system to start the manufacture of the required defensive antibodies and white cells. In this way the body is pre-prepared for an actual invasion and it can destroy the viruses before they can cause the illness. This process is usually called vaccination or (artificial) immunization.
Producing a vaccine that will boost the immune system to fight four different types of dengue virus has proved particularly difficult. Vaccines for all four serotypes are not likely to be available for a few years, although some are presently being tested. In the meantime, the only control of dengue is through the effective control of the mosquitoes.
Severe haemorrhage or not
There has been some evidence indicating that dengue with severe bleeding was more likely during a second dengue infection than during a first infection. It was thought that the first infection caused a process in the immunity system than actually enhanced the next dengue infection. However, for our area at least, recent research in Tahiti has concluded that dengue with severe bleeding was as likely during a primary infection as a secondary infection.
In the 1980s the Asian experience indicated that Dengue-2 and Dengue-3 were more often associated with severe haemorrhage and it was suggested that these might be the more virulent types. However experience since then has shown that severe haemorrhage can be associated with any of the four types.
The Pacific experience with dengue has provided important information related to the occurrence of dengue with severe haemorrhage. In the early 1970s there was a widespread outbreak of Dengue-2 in the South Pacific and it was non-fatal, except in Tahiti and Niue. It hit Niue in 1972 and caused several deaths among young people who had not previously had dengue. It was also noticed that most of the severe cases occurred in the second half of the epidemic. All four types of dengue (1 thru 4) can cause an infection ranging from one without any obvious symptoms, through the painful classical Dengue Fever (DF), to the severe bleeding of Dengue Haemorrhagic Dengue (DHF), which can put the circulatory system into life-threatening stress, a condition known as Dengue Shock Syndrome (DSS).
Researchers in Tahiti concluded that the severity of the illness is related to “the interactions of several factors related to the virus, to the host, and to the vector”. This basically means that, at present, scientists have very little idea why some patients develop severe haemorrhagic symptoms. It is still unpredictable and all that can be done is to monitor the progress of the illness in each patient with care - and take appropriate action.
Symptoms and disease names
Dengue Fever (DF) involves at least two of the following symptoms: high fever (for 2-7 days, usually 6-7, and sometimes having two peaks), intense headache, painful eye-movement, intense muscle or joint pain, and body rash. In children DF is usually mild, while adults can have more extreme bone pain and recovery can involve prolonged fatigue and depression. Classical Dengue Fever can involve mild bleeding: indicated by scattered blood spots in the skin.
Technically blood samples, called sera, can be tested to determine if you have serotype Dengue-1, -2, -3 or -4. But as outlined above, the type is not considered significant as to the likelihood of it developing into serious haemorrhage. A more useful test to determine that you have dengue, and not another type of illness, is to measure the concentration of platelets - the clotting cells - in your blood. Normally you have 200,000-500,000 platelets per millilitre and a decrease to less than 100,000/mm² is often used as a positive indicator of dengue.
The best treatment is rest, lots of fluids or rehydration drinks, while reducing the fever and pain with paracetamol (NEVER asprin and NEVER brufen because these encourage bleeding). Paracetamol (also known as acetominophen,) is sold under various trade names, including Panadol and Panadeine. Be friendly to your liver by not taking more than the recommended maximum dosage and by avoiding alcohol.
For those not under detailed medical supervision it is very important during the fever, and during the two or three days of recovery, to watch for any sudden deterioration - frequent checking is important! Immediate hospitalisation is essential if any of the following are noticed: bleeding into the skin or from the nose or gums, abdominal pain, black stools, excessive sweating, bluish lips, or cold and clammy skin. These are signs of severe internal bleeding and plasma leakage and they indicate that intravenous therapy is required immediately. The therapy required will vary from intravenous fluids (also called electrolyte or crystalloid), to colloid or plasma (without or with platelet concentrate), to whole blood.
WHO developed a classification of dengue illnesses based on the severity of the symptoms. (1) Dengue Fever (DF) without haemorrhage, and DF with “usual” haemorrhage - the latter is sometimes called haemorrhagic dengue. (2) Dengue Haemorrhagic Fever (DHF) with severe haemorrhage with four grades, the two most severe grades also being referred to as Dengue Shock Syndrome (DSS).
The severe Dengue Haemorrhagic Fever (DHF) was identified by two key indicators: a platelet count of less than 100,000/mm², and evidence of plasma leakage. DHF grades 1 and 2 involved evidence of internal bleeding. The initial stage of shock is in Grade III with weak and rapid pulse, low blood pressure (hypotension) and restlessness; while Grade IV is profound shock with undetectable pulse and blood pressure.
Although WHO defined DF and DHF to assist in the accurate reporting of dengue outbreaks, there is a reluctance by countries to refer to Dengue Haemorrhagic Fever, because it increases fear within the community and the travelling public. Despite the fact that the fatality rate of managed Dengue Haemorrhagic Fever is extremely low, the mere mention of the word Haemorrhagic Fever generates images of a high death rate. This situation has made health providers reluctant to use the WHO classification system in public, which leaves the public guessing as to whether severe haemorrhage is a likely within the present epidemic. You should therefore assume that severe haemorrhage is always a possibility with Dengue Fever. Seek medical advise or, at least, be very vigilant for signs of bleeding.
Cook Islands Epidemics
Several South Pacific island countries had Dengue-1 outbreaks in the 1930s and again in the 1940s. All epidemics were of the mild classical form, and Rarotonga had its outbreak in 1946. At the time the island had Aedes aegypti and Aedes polynesiensis, and the first was assumed to be the vector. In 1946 Dr Tom Davis implemented mosquito controls to reduce filariasis spread by Aedes polynesiensis, and as a by-product Aedes aegypti was eradicated some time before a 1955 survey.
In 1964 the Society Islands had an epidemic of Dengue-3, and in 1971-72 several island countries had Dengue-2 epidemics. Although they all presumably got the same virus, the disease caused some severe haemorrhage in Tahiti and Niue, but it was mild in Fiji, Samoa and elsewhere. The Cook Islands missed out.
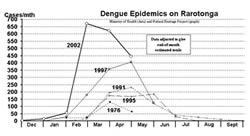 There was a widespread outbreak of Dengue-1 in 1975-76, with some severe haemorrhage in Tonga and Niue, but mild in Tahiti, Samoa and Fiji. This epidemic came to Rarotonga in December 1975 with a Tahitian football team, and the local epidemic was especially widespread during March and April 1976 (see the graph). By the end of April 254 people had been treated for dengue, and home surveys indicated that the actual number with clinical symptoms of dengue was about four times the number treated. That meant that about 1000 people had dengue with the usual clinical symptoms. The epidemic was of the milder classical Dengue Fever without any sign of severe haemorrhage. The Tahitian footballers also visited Aitutaki and that island eventually reported 153 cases of dengue.
There was a widespread outbreak of Dengue-1 in 1975-76, with some severe haemorrhage in Tonga and Niue, but mild in Tahiti, Samoa and Fiji. This epidemic came to Rarotonga in December 1975 with a Tahitian football team, and the local epidemic was especially widespread during March and April 1976 (see the graph). By the end of April 254 people had been treated for dengue, and home surveys indicated that the actual number with clinical symptoms of dengue was about four times the number treated. That meant that about 1000 people had dengue with the usual clinical symptoms. The epidemic was of the milder classical Dengue Fever without any sign of severe haemorrhage. The Tahitian footballers also visited Aitutaki and that island eventually reported 153 cases of dengue.
In 1974, 500 school children who had not been off-island were tested and only two (0.4%) had dengue antibodies. In March 1976, three months into the epidemic, 70 Ngātangi‘ia children who had had no noticeable signs of dengue were tested and 77% had dengue antibodies. This indicated that a large proportion of people on the island probably had had a very mild infection of dengue and would have become immune to that serotype.
The 1975 epidemic was of interest because no Aedes aegypti were found on the island. It was concluded that the virus was successfully spread by Aedes polynesiensis, although later experiments showed it to be a much less efficient vector than Aedes aegypti.
1979-80 saw Dengue-4 in Tahiti, the first time this serotype occurred outside Asia. It was generally mild, although one child died of serious haemorrhage. It spread to several other countries where it was not associated with fatalities, although it slammed Niue with three fatalities and 700 people required medical treatment. The Cook Islands did not have an epidemic, although there may have been a few cases.
There were a variety of outbreaks around 1990. Tahiti had an epidemic of Dengue-1 in 1988-89, followed immediately by a Dengue-3 epidemic in 1989-90. In 1991 the Cook Islands was hit hard by a Dengue-1 epidemic with some severe haemorrhage. As the graph shows the epidemic peaked in April. In all there were 550 reported cases, and of these 20% (98) were classified as having had Dengue Haemorrhagic Fever because their platelet count was less than 100,000/mm², and of these 80% had direct evidence of internal bleeding. The DHF patients ranged from five to seventy years, with most in the 15-24 age group. There was no sex predominance. Three patients died before platelet concentrate became available on 11th April, and subsequently 51 patients were given plasma with platelet concentrate and all recovered. In one unusual case a patient with a platelet count of 7,000/mm² recovered after receiving intravenous fluids alone without plasma or platelets.
The outbreak was severe on Mangaia with no fatalities, and severe on Aitutaki with two fatalities. The outbreak on Manihiki was also severe.
A year later, in November 1991, Aedes aegypti was recorded on Manihiki. During 1993 and '94, Dr Ichimori re-affirmed aegypti on Manihiki, and also found it on Penrhyn and Rarotonga, where it was widespread on the north side with one site in Tïtīkāveka. How long it had been on these islands is unknown, and the sequence of invasion is also unknown.
The next Cook Islands outbreak was in 1995, introduced from Fiji. It was not associated with fatalities. The epidemic itself had a similar profile to the 1991 epidemic, with the peak in April.
1996-97 saw a Dengue-2 epidemic in Tahiti, and the Cook Islands joined in with it biggest dengue epidemic in early 1997. This epidemic rose rapidly during February and March to reach its peak in April - and then it crashed. No fatalities.
Dengue-1 was common in Samoa and Tahiti during 2001 and by mid-year a few visitors and returnees were bringing it to Rarotonga. There was no epidemic, presumably because the mosquito concentration was too low to launch it. However, with the arrival of summer warmth and rains there was a great increase in mosquitoes and the epidemic was successfully launched by visitors from Tahiti in late November. The rise in cases was extremely dramatic during February. Increased awareness on household mosquito control and mass spraying around dwellings of infected people were not sufficient to halt the epidemic. To reduce the level and duration of the epidemic Operation Namu was launched on 22nd February. This programme has involved extensive clearing of overgrown sections near dwellings, and widespread fogging of the lowland with malathion and, later, the pyrethoid Reslin. It will be sometime before Government is able to provide a scientific analysis of the medical nature of this particular epidemic and the effects of Operation Namu. This knowledge will assist in the handling of future epidemics.
An overview of the five recent dengue epidemics in the Cook Islands shows a strong summer pattern. The epidemics typically start with viruses imported from Tahiti during December or January, and after a month of low activity there is a dramatic increase. The peak levels of infection last two or three months, followed by a rapid collapse. It is interesting that the two latest epidemics grew a month earlier, grew much faster, and reached greater heights than the previous three.
Tahiti |
Rarotonga |
|||
Serotype |
Year |
Cases |
Year |
Cases |
Dengue-3 |
1964-65 |
1,358 |
- |
- |
Dengue-3 |
1969 |
72 |
- |
- |
Dengue-2 |
1971 |
12,943 |
- |
- |
Dengue-1 |
1975-76 |
2,032 |
1976 |
330 |
Dengue-4 |
1979 |
7,489 |
- |
|
Dengue-1 |
1988-89 |
6,232 |
1991 |
641 |
Dengue-3 |
1989-90 |
6,534 |
- |
- |
Dengue-3 |
- |
- |
1995* |
583 |
Dengue-2 |
1996-97 |
7,465 |
1997 |
1,200 |
Dengue-1 |
2001-02 |
? |
2002 |
? |
| * the 1995 epidemic was introduced from Fiji. | ||||
First published in the Cook Islands News, 9 March 2002
About Gerald McCormack
 Gerald McCormack has worked for the Cook Islands Government since 1980. In 1990 he became the director and researcher for the Cook Islands Natural Heritage Project - a Trust since 1999.
He is the lead developer of the Biodiversity Database, which is based on information from local and overseas experts, fieldwork and library research. He is an accomplished photographer.
Gerald McCormack has worked for the Cook Islands Government since 1980. In 1990 he became the director and researcher for the Cook Islands Natural Heritage Project - a Trust since 1999.
He is the lead developer of the Biodiversity Database, which is based on information from local and overseas experts, fieldwork and library research. He is an accomplished photographer.
Citation Information
McCormack, Gerald (2005) Dengue - A Complex Disease. Cook Islands Natural Heritage Trust, Rarotonga. Online at http://cookislands.bishopmuseum.org. ![]()
Please refer to our use policy
